Things have been about as medically quiet as
they get for me. That doesn’t mean no complications, but it does mean nothing particularly
dire. One frustrating thing is that I’ve had continuous lung infections since
finishing IV antibiotics. In March I cultured staph, but fortunately it was an
easily treatable one that was resolved with oral antibiotics. Then in April I
cultured my old nemesis pseudomonas. I haven’t had much in the way of symptoms
however, so we haven’t jumped into any drastic treatments yet. I already do a
nebulized antibiotic on a 1 month on, 1 month off schedule, and April was my
off month, so as long as I remain mostly symptom free we’ll just see if it clears
up by the end of May. I’m also having an appointment with my ENT to see if
there’s anything else we can do with my miserable sinuses to keep the infections
from dripping down into my lungs.
The main symptom I’ve had is fatigue, but it’s
hard to tell how much of that is from the infection and how much is just my
life. I’ve struggled with poor sleep for decades, but I definitely feel like it
got worse after transplant, so that obviously contributes to fatigue. I think I’ve
heard that insomnia and fatigue aren’t uncommon after transplant, so it could
just be transplant life. And I’m sure battling a pseudomonas infection doesn’t
help. All I know is that I’ve been VERY tired lately, which makes it really
difficult to get anything done and kinda sucks the life out of me. Here’s
hoping that improves along with the pseudomonas infection.
I also had my first post-transplant dermatology
appointment. You’re supposed to have one every year after transplant, but due
to Covid we pushed off most non-essential appointments. Penn now has a special
transplant dermatology program though, and they’re good about making sure we
all get in to see them. I knew that transplant recipients are at higher risk
for all kinds of cancers, but I didn’t realize that the risk of skin cancers in
particular is ridiculously high. Thankfully my skin looked good this time, but
the doctor said that 3-5 years after transplant is when they typically start
seeing skin cancers. And guess whose 3 year lungiversary is this week?? So that’s
another worry to add to my long list of fears. I’ll definitely be more cautious
about covering up and using sunscreen!
On the non-medical front, we unfortunately have
some sad news. After having a bad fall last summer and then struggling for
months with one medical issue after the next, Katherine’s mother passed away
last month. It was a strange mix of unexpected and expected: unexpected,
because before the fall she was doing fine, and expected, because she declined
for months before finally being sent home on hospice. Things were pretty awful
at the end, and it was a mercy when she finally passed. It’s been difficult,
but Katherine is holding up ok, and we all hope her mother is finally at peace.
On a brighter note, I’ve really been appreciating
being able to get out and socialize a bit instead of being on full Covid
lockdown. I went out for half of the holiday meals on Pesach, which was AMAZING
and made the holiday SO much more enjoyable. I’ve also been going out for some
Shabbos meals. And in an effort to get some exercise, I started taking lessons
with my friend Abrielle Fuerst, who teaches martial arts professionally. So
that’s guaranteed once a week that I get out of the house and see a friend, and
I get to learn how to be a ninja on top of it! I am playing with NUNCHUCKS,
people! Watch out!
The experiences, thoughts, and ramblings of an adult with Cystic Fibrosis.
Showing posts with label exercise. Show all posts
Showing posts with label exercise. Show all posts
Monday, May 9, 2022
Thursday, November 21, 2019
Donor Dash!
Current goal: do the real Donor Dash this year instead of the inpatient version! Time to start training!!
Also, if anyone wants to see last year's inpatient donor dash, I actually recorded it for posterity: https://youtu.be/t7tZO8gqt0Y
Wednesday, August 21, 2019
3 month bronchoscopy!
Check out https://youtu.be/W1pQaEHWdDk if you’d
like to see a video recap of bronchoscopy day!
Thursday was my big bronchoscopy
day! Post-transplant it’s standard to have bronchoscopies after 6 weeks, 3
months, 6 months, and 1 year, and then annually after that. During a bronchoscopy
they put a scope down my throat and into my lungs to look around and make sure
everything is ok, and take sputum samples and biopsies to check for infection
and rejection. In my case, we already knew things weren’t 100% perfect and that
they’d have to open up and clear out some airways. Thankfully, I’m under
general anesthesia for this whole process. General anesthesia used to be a big
scary deal with my old lungs, but seems to be a lot easier and more standard
with my shiny new ones. So on Thursday I went to HUP, changed into my very
fashionable hospital gown, and went to sleep for a few hours while they fixed
me up.
My biggest problem
post-bronchoscopy is usually that my throat is very sore and it’s difficult to
eat. This time we came prepared with a quart of Rita’s water ice in a cooler so
I’d have something cold and delicious to soothe my throat. The nurses and other
patients in the recovery room were quite impressed with our foresight and
planning! Katherine also continued our new tradition of getting a cute little
stuffed animal from the gift shop for me to wake up to post-bronchoscopy. So far
there are two, and I’m calling them the Bronchoscopy Collection. At least now I
have something fun to look forward to each time!
Shortly after the procedure they
let us know that a few airways had been narrowed on the right side and one was
narrow on the left side, so they went in and inflated a balloon to open and
widen them. There was also necrotic tissue blocking some airways on the right
side, which sounds scary but apparently is common. They saw the same thing
during my previous bronchoscopy, and both times they were able to remove the
dead tissue and open up the airways. I’m wheezing a lot less now, though I’m
still a bit congested as I clear out the mucus that was trapped during the last
several weeks. Hopefully things will heal up and clear out by the time I see
the doctor again in 2 weeks, and my pulmonary function numbers will go way up!
Today I got my test results from
the sputum samples and biopsies, and the verdict is… no infection and no
rejection! We didn’t get cake this time, but it’s very exciting and encouraging
that things continue to go so well! Now I just need to get the hip pain under
control so I can get back on track with my exercise routine and rebuild my strength
and endurance. I’m also still having some pain in my incisions, though it’s gotten
MUCH better. Katherine keeps reminding me that it’s only been 3 months, and
that I need to relax and not push myself too hard. Which is hard when I’m
feeling SO much better and more capable. I want to conquer the world NOW!
Fiiiine, I guess I’ll try to cut
myself some slack and allow this process unfold at its own pace – but I WILL
get these lungs back up to 80% and beyond! Just you wait and see!!
Friday, July 19, 2019
Graduation!
Officially graduated from pulmonary rehab! But the hard work continues as now I need to keep up with a home exercise program to maintain my progress. For now though, we're celebrating with cake!
Sunday, April 28, 2019
Thursday, March 14, 2019
Keeping on keeping on
Welp, I managed to regain a whole 1%
in lung function. Go me.
I am feeling a little better. My
oxygen has been a little more stable and my heart rate hasn’t been going quite
as high with exertion, though I do still need some supplemental oxygen when I’m
out and about. I’ve also been a little less congested. Overall though the gains
haven’t been too significant, so much to my disappointment my doctor wants to
try one more week of IV antibiotics. Thankfully, however, we’re stopping the
Zosyn and switching me back to Zerbaxa, aka the Fancy Restricted Antibiotic.
This is so that I can get a LITTLE more sleep, since Zosyn is run every 6 hours,
whereas Zerbaxa is run every 8 hours. I’ve been an utterly sleep deprived zombie
these last couple weeks, so at this point I’ll take whatever I can get! I feel
like a cat these days: I don’t actually sleep anymore, I just take naps of varying
lengths at various points throughout the day. I think cats enjoy this more than
I do though!
On the plus side, my last sputum
culture did NOT show MRSA or either of the two fungal infections that popped up
previously. Unfortunately, that hasn’t actually translated into any real improvement
in my health. If I don’t see any real improvement with another week of IV antibiotics,
we’re going to move on to treating the other infection that has been cropping
up lately in my sputum cultures: mycobacterium chelonae, a nontuberculosis
mycobacterium (aka NTM). We haven’t treated it until now because it’s unclear
whether the NTM is actually the source of any of my symptoms, and treating it
requires taking multiple antibiotics for a very extended period of time. Apparently
it can also be difficult to get approval for some of the medications involved.
And, one of the meds used to treat it is Tobramycin, the IV antibiotic which
gave me tinnitus and can cause hearing loss. We’re exploring whether I can take
the Tobra via nebulizer, which has less risk of causing hearing issues, but unfortunately
in the past the nebulizer formulation of Tobra (called TOBI) gave me asthma
attacks. I’ve asked whether we can try giving me the IV version of Tobra to
inhale, which is what I did for years without any problems before TOBI was
developed. It’s unclear however whether we’ll be able to get approval for an
off-brand use of injectable Tobra since a nebulizer version is available.
The other main goal now is getting me
to be a little more active. I’ve been feeling sort of awful both physically and
mentally, which has led to me spending a LOT of time moping on the couch. I’m
trying to pull myself together and leave the house a little more, even if only
briefly, and to do brief, mild exercise at home a few times a day. I’m
obviously not running any marathons, but whatever exercise I can manage is good
for both my physical and mental health. I just need to be careful about not
pushing my heart rate too high, as unfortunately the “leaky pipes” have still
been an issue. Thankfully I haven’t had a full bleed in two and a half weeks,
but I’ve been having varying degrees of bloody mucus at least once a week all
month. I’m trying really hard to avoid anything that could trigger a full
bleed, as that would force me to hold various treatments and prevent me from
clearing mucus out of my lungs. On the other hand, I do need to exercise,
because not exercising is also detrimental to my lungs as well as the rest of
my body. It’s a really fun catch-22.
It has been a really, really
difficult winter. Hopefully things will start looking up soon.
Tuesday, August 7, 2018
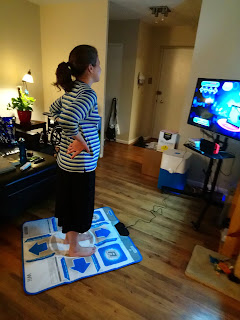
Dance therapy
Who needs pulmonary rehab when you have Dance Dance Revolution? I had to give up after the second round though when my oxygen started dropping. It's a work in progress! Also, we've officially found a game where Katherine wipes the floor with me lol!
Subscribe to:
Posts (Atom)